The Meaning Of Life Is That It Stops
The new IT article on health care: How American Health Care Killed My Father, by David Goldhill, writing in the September 2009 Atlantic.
Richard Dooling on NPR’s Talk of the Nation discussing his opinion piece in the New York Times, “Heath Care’s Generation Gap.“
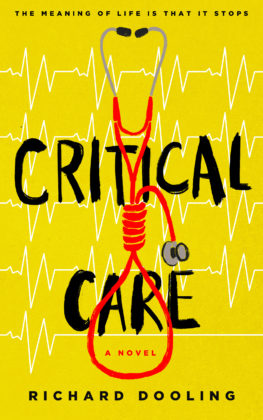
It was my first novel, and I wrote it almost two decades ago, but I doubt I’d change a word of it. If anything, the money and the madness changing hands in the ICU have only gotten worse. When I wrote Critical Care, circa 1990, total expenditures for health care ran at roughly 10% of our gross national product. Now, as my opinion piece in the New York Times indicates, it’s 16% and headed for 31% in the next 25 years, unless something changes.
The new hysterical fear is that if we counsel elderly patients about end-of-life choices it means we are “pulling the plug” or sending them off to suicide parlors. People need to know what all of this aggressive, no-holds-barred, spare-no-expense intensive care buys you at the end of life. It’s not pretty, and that is the real subject of Critical Care: What happens when modern medicine doesn’t know when to quit.
Here then, by popular demand, is an excerpt from an early chapter of Critical Care: A Novel:
Code Blue
Resignation was the order of the day. Everybody from the nurses on down to the respiratory therapists and the lab techs had already privately agreed that Bed One would ‘code’ sometime tonight, code being short for Code Blue. Bed One’s heart would stop beating, or he would stop breathing, or both; the hospital operator would then announce: “Code Blue, Ninth Floor Intensive Care Unit” three times over the hospital’s public address system, and a dozen or so specially trained personnel would then descend on Bed One, snap Bed One’s head back, pump Bed One’s lungs full of oxygen with an ambu bag, inject massive doses of expensive drugs in some of Bed One’s veins, draw blood for expensive tests from other veins, shock Bed One with electricity, beat on Bed One’s chest, and generally do everything possible to jump-start Bed One, as if Bed One were a ’57 Chevy that should have been taken to the junkyard twenty years ago, and the doctors and nurses were a bunch of drunk teenagers whose car had broken down on the way to a pig roast.
It would go on for hours. It would require more blood, stool, and sputum specimens to be drawn and sent to the lab. Worse yet, everything would have to be scrupulously documented for the Legal Department. Afterwards, there would be witness interviews, probably depositions, just like the ones they had after the craniotomy in Bed Seven was struck by lightning that came in through the TV set.
Bed One had no business dying from a simple valve replacement. The lawyers knew that.
Because it was 3:30 A.M., Werner was solely responsible for the likes of Bed One. All the real doctors and primary physicians had gone home, had barbecued steaks, had watched a few hours of cable TV and had gone to bed. In Werner’s capacity as House Officer, Werner had to respond to every medical emergency occurring outside the normal hours of the medical work day: like Bed One dying too soon.
“This is what makes it all worthwhile,” he said to a wombat at his elbow. “Being able to help people. This is where training pays off.”
Werner looked the impending medical crisis squarely in the eye and measured himself against it, his self-confidence barely surmounting sleepless anxiety. As usual, he fought the urge to panic by silently reminding himself of his credentials: I am Doctor Peter Werner Ernst. I graduated at the top of my medical school class. I was Editor-In-Chief of the University’s Journal of Medicine. I am qualified and capable of practicing medicine. I will not panic or succumb to stress and make the wrong decision. That would be irrational and inconsistent with my past performance.
Given the hopelessness of Bed One’s situation, another medical resident might have thrown up his hands and accepted the inevitable descent of the patient. Another resident might have been discouraged by the resignation on the faces of the Intensive Care Unit nurses–faces that said ‘Bed One is about to code, creating boatloads of pointless labor and paperwork for us all.’ Yes, another resident might have allowed the normal course of human events to degenerate into chaos, death, and a Code Blue. But not Werner Ernst. Werner was blessed with a superior medical mind, trained in the healing arts.
Werner’s rigorous training had prepared him for this moment, when he, the House Officer in charge of the Medical Center and the resident physician immediately responsible for the welfare of Bed One, would come up with the right combination of medications to drip into Bed One, just the right mix of dosages given at just the right intervals, to keep blood pressure up, keep CO2 down, keep heart beats passably even, and urine flowing . . . keep everything just so, for six or seven hours at least . . . so that Bed One would go down the tubes and croak on the Day Shift, not the Night Shift. So that Werner could eat and possibly nap tonight, instead of presiding over the death of a corpse. So that the ICU nursing staff could embroider or read romance novels through the wee hours. So that Bed One could sleep one, last, peaceful, vegetable sleep before being assaulted by a Code Blue wrecking crew trying to save his life. And, above all, so that all the wicked, ridiculous insanity concerning the demise of Bed One (who, only two months ago was a grandpa, a loving husband, and dad to the people who had brought him here) would come down on Bed One’s primary physician and the Day shift. The Day Shift had advised Bed One and Bed One’s family that eighty was not too old to try for another valve replacement. Eighty? Bed One’s primary physician, Bed One’s chest surgeon, and Bed One’s family made Bed One’s bed of slaughter and anguish, why should Werner and the Night Shift sleep in it?
Excerpted from Critical Care: A Novel, by Richard Dooling
